Monday, August 13, 2007
In Reply to: Gastroparesis meds-what do you use?
Jerry took reglan, propulsid. none worked like this:::: erythromyacin liquid. 1/8th teaspoon before meals. the side effects of this antibiotic they have found will cause motility (cramping)but very mild,since you are using it theraputically , not as an antibiotic.
NOW youll be hard pressed to find any info on gastroparesis that doesnt involve diabetes. it doesnt matter because the symptoms/treatments are the same. It is all damage to the vagus nerve.
Gastroparesis doesn't sound good, and it isn't. Literally "stomach paralysis," it is a form of diabetic neuropathy, or nerve damage, that is a common complication of diabetes. The damaged nerve in question is the vagus nerve, named for its vagabond-like wandering nature.
The vagus nerve meanders all the way from the brainstem to the colon, controlling heart rate, sweating, gastrointestinal contractions, and various other involuntary, automatic functions on its way. In the case of gastroparesis, it's the vagus nerve's control of stomach contractions that's damaged.
The stomach is basically a hollow ball made of muscle that serves as a storage container and mixing bowl for food. It's about the size of a small melon, but it can stretch to hold nearly a gallon if you really press the issue. In healthy people, wave-like contractions of the stomach, prompted by the vagus nerve, crush and churn your food into small particles and mix it up with enzymes and acids produced by the stomach's inner lining.
Then the stomach contractions, coming along in waves at about three per minute, slowly and evenly propel the pulverized food out through the pyloric valve, which opens just enough to release an eighth of an ounce of food at a time. From there it's down the small intestine, where the real nutrient absorption occurs. It can take four hours to empty your stomach into your small intestine, especially if you've eaten fat, which slows the process down.
If the vagus nerve has been damaged by years of high blood sugars, the process hits a snag. The walls of the stomach, paralyzed by the lack of vagus nerve stimulation, don't make their muscular wave-like contractions. As a result, food just sticks around in the stomach, unpulverized and going nowhere. It may sit and ferment, creating an environment that fosters the growth of harmful bacteria.
Alternatively, the food can harden into solid masses called bezoars (pronounced "bee's oars") that are similar to a cat's hairball. In olden days, bezoars were thought to be magical poison antidotes and were worth several times their weight in gold. These days, however, all they do is cause nausea and vomiting. Worst case scenario, they can even block the pyloric valve, creating a serious emergency.
The common symptoms of gastroparesis are bloating, abdominal pain, nausea, feeling full after just a few bites of a meal, weight loss, and heartburn. Nausea and vomiting generally occur many hours after the last meal, usually when your stomach is fullest from both food and the secretions stimulated by the food. Because the food hasn't been ground up during the interim, it often comes up in the same shape it went down in, so it is, unpleasantly enough, easily recognized.
Diabetes is the leading risk factor for gastroparesis. About one in five people with type 1 develop it, as well as many people with type 2. Once it develops, it makes blood sugar management even harder because erratic stomach emptying make blood sugar levels difficult to predict and control. Conversely, poor control of blood sugar levels makes gastroparesis worse by tending to slow gastric emptying.
There are any number of new methods to look for gastroparesis, many of which involve eating or drinking something rather unappetizing. In a gastric emptying study, considered one of the most accurate methods to diagnose gastroparesis, you must eat eggs or oatmeal containing a harmless radioactive substance that makes the food visible on a Geiger-counter-like scan. Less commonly, you might undergo a barium x-ray, in which you fast for twelve hours and then drink a sludgy liquid that coats the inside of your stomach and makes its contents visible on x-ray.
Other diagnostic tests involve threading a little tube down into your stomach to assess the strength, frequency, and coordination of your stomach contractions or the electrical signals that travel through your stomach and stimulate its contractions.
The simplest way to address gastroparesis is through dietary changes. Smaller, more frequent meals ameliorate that feeling of fullness and are faster and easier to digest than three big meals. If your appetite diminishes later in the day, eat more in the morning and stick to liquids in the afternoon. By lying on your right side after eating, you can put gravity to work to help empty your stomach.
A big problem is fiber, which helps things move along in the intestines but has the opposite effect in the stomach. The stomach has a hard time breaking down roughage, which is also more likely to sit around and form those unwanted bezoars. So people with gastroparesis are often advised to avoid raw vegetables and eat soft, low-fiber foods like well-cooked fruits and vegetables, fish, chicken, yogurt, refined breads and grains, or pureed or liquid foods.
Sometimes it's advisable to avoid fats, which slow down stomach emptying even in healthy people. If you're vomiting a lot, it's also important to drink water to avoid dehydration and to take supplements in liquid form. If you can't tolerate any food or liquid at all, your doctor might place a feeding tube in your small intestine to bypass your stomach altogether. It's usually a temporary fix, used only in severe cases or when blood sugar levels can't be controlled.
Sometimes gastroparesis can be worsened, or even caused, by medications that slow stomach emptying, including narcotic pain medications, tricyclic anti-depressants, and calcium channel blockers, as well as some blood pressure medications, lithium, and antacids that contain aluminum hydroxide.
Clonidine, dopamine agonists, and progesterone are also implicated. So if you have gastroparesis, your symptoms could improve if you move off those medications under the care of your doctor. Nicotine is also associated with impaired gastric emptying, so you might want to quit smoking.
Especially in people with diabetes, it's critical to regain control of blood sugar levels that are out of whack, especially because better control of blood sugar levels can actually improve stomach emptying. Sometimes it can help to take insulin after meals instead of before. Testing more frequently will allow you to take insulin in response to blood glucose levels as they rise, rather than in response to a meal that might just take awhile to hit the bloodstream. Your doctor can advise you about methods to bring your blood sugars down and, hopefully, relieve your gastroparesis.
There are a number of drugs available to treat gastroparesis: Some of them relieve nausea and vomiting; others ease abdominal pain. Others still, called pro-motility drugs, stimulate contractions of the stomach muscles. There's also the rather new possibility of getting a pacemaker for your stomach, which generates electrical pulses that stimulate the wave-like muscle contractions you need to get things moving again.
The latest (and still experimental) treatment is injection of botulinum toxin (Botox) into the pylorus; just like it does to your forehead wrinkles, the Botox temporarily relaxes the powerful pyloric muscle, thereby enlarging the outlet from the stomach to the intestine and allowing the release of more food.
Gastroparesis is not usually life-threatening, but it can really put a dent in your quality of life and make your diabetes much harder to control. There's been a lot of progress made recently in treatments for the condition, so think about taking a trip to your doctor or gastroenterologist. It just might get things moving along in the right direction. www.diabeteshealth.com/read/2007/06/30/5283.html
GastroparesisMedical Revising Author: Dennis Lee, MD Medical Revising Editor: Jay W. Marks, MD
What is gastroparesis? What are gastroparesis symptoms and signs? What causes gastroparesis? How is gastroparesis diagnosed? How is gastroparesis treated? What is the prognosis (long-term outcome) for patients with gastroparesis? What's new in gastroparesis? Gastroparesis At A Glance What is gastroparesis?
Gastroparesis means paralysis of the muscles of the stomach. Gastroparesis results in delayed emptying of food from the stomach into the small intestine.
The stomach is a hollow organ composed primarily of muscle that serves as a storage container for food. Food in the stomach is ground into tiny pieces by the constant churning that is generated by the contractions of the stomach’s muscles. Once the food has been adequately ground, it slowly is emptied from the stomach into the intestine in a metered fashion. Only food ground into small particles can be emptied from the stomach in a normal fashion, and smaller particles are digested better in the intestine. Moreover, the metering process allows the emptied food to be well-mixed with the digestive juices of the intestine, pancreas, and liver (bile) and to be absorbed well from the intestine.
When the stomach’s muscles are paralyzed, food is not thoroughly ground and does not empty into the intestine normally. Since the muscular mechanisms whereby ground, solid food and liquid food are emptied from the stomach are different, there may be delayed emptying of solid food (most common), solid and liquid food (less common), or liquid food alone (least common).
What are gastroparesis symptoms and signs?
The primary symptoms of gastroparesis are nausea and vomiting. Other symptoms of gastroparesis include abdominal pain, bloating, early satiety (feeling full quickly when eating), and in severe cases, weight loss due to a reduced intake of food because of the symptoms. Reduced intake of food and restriction of the types of food that are eaten can lead to nutritional deficiencies.
The vomiting of gastroparesis usually occurs after meals; however, with severe gastroparesis, vomiting may occur without eating due simply to the accumulation of secretions in the stomach. The characteristic vomiting happens several hours after a meal when the stomach is maximally distended by the presence of food and secretions stimulated by the meal. Since the grinding action of the stomach is absent, the vomited food often remains in larger pieces and is easily recognized. (Contrast this with the more common type of vomiting in which the food appears as small, uniform, unidentifiable particles.)
Other, less frequent effects of gastroparesis are the promotion of gastroesophageal reflux disease (GERD) and malnutrition.
What causes gastroparesis?
Gastroparesis can be caused either by diseases of the stomach’s muscles or the nerves that control the muscles, though often no specific cause is identified. The most common disease causing gastroparesis is diabetes mellitus which damages the nerves controlling the stomach muscles. Gastroparesis also can also result from damage to the vagus nerve, the nerve that controls the stomach’s muscles, that occurs during surgery on the esophagus and stomach. Scleroderma is an example of a disease in which gastroparesis is due to damage to the stomach’s muscles. Occasionally, gastroparesis is caused by nervous reflexes, for example, when the pancreas is inflamed (pancreatitis). In such cases, neither the nerves nor the muscles are diseased, but messages are sent through nerves from the pancreas to the stomach which prevents the muscles from working normally.
Other causes of gastroparesis include imbalances of minerals in the blood such as potassium, calcium or magnesium, medications (such as narcotic pain-relievers), and thyroid disease.
Gastroparesis can occur as an isolated problem or it can be associated with paralysis of other parts of the intestine, including the esophagus, small intestine, and colon.
How is gastroparesis diagnosed?
The most common method for diagnosing gastroparesis is a nuclear medicine test called a gastric emptying study which measures the emptying of food from the stomach. For this study, a patient eats a meal in which the solid food, liquid food, or both contain a small amount of radioactive material. A scanner (acting like a Geiger counter) is placed over the stomach for several hours to monitor the amount of radioactivity in the stomach. In patients with gastroparesis, the food takes longer than normal (usually more than several hours) to empty into the intestine.
The antro-duodenal motility study is a study that can be considered experimental that is reserved for selected patients. An antro-duodenal motility study measures the pressure that is generated by the contractions of the muscles of the stomach and intestine. This study is conducted by passing a thin tube through the nose, down the esophagus, through the stomach and into the small intestine. With this tube, the strength of the contractions of the muscles of the stomach and small intestine can be measured at rest and following a meal. In most patients with gastroparesis, food (which normally causes the stomach to contract vigorously) causes either infrequent contractions (if the nerves are diseased) or only very weak contractions (if the muscle is diseased). An electrogastrogram, another experimental study that sometimes is done in patients with suspected gastroparesis, is similar to an electrocardiogram (EKG) of the heart. The electrogastrogram is a recording of the electrical signals that travel through the stomach muscles and control the muscles' contractions. An electrogastrogram is performed by taping several electrodes onto a patient's abdomen over the stomach area in the same manner as electrodes are placed on the chest for an EKG. The electrical signals are recorded at rest and after a meal. In normal individuals, there is a regular electrical rhythm just as in the heart, and the power (voltage) of the electrical current increases after the meal. In most patients with gastroparesis, the rhythm is not normal or there is no increase in electrical power after the meal. Although the gastric emptying study is the primary test for diagnosing gastroparesis, there are patients with gastroparesis who have a normal gastric emptying study but an abnormal electrogastrogram. Therefore, the electrogastrogram is useful clinically primarily when the suspicion for gastroparesis is high but the gastric emptying study is normal or borderline abnormal.
A physical obstruction to the emptying of the stomach, for example, a tumor that compresses the outlet from the stomach or scarring from an ulcer, may cause symptoms that are similar to gastroparesis. Therefore, an upper gastrointestinal (GI) endoscopy test usually is performed to exclude the possibility of an obstruction as the cause of a patient's symptoms. (Upper GI endoscopy involves the swallowing of a tube with a camera on the end and can be used to visually examine the stomach and duodenum and take biopsies.)
Upper GI endoscopy also may be useful for diagnosing one of the complications of gastroparesis, a bezoar. Because of the poor emptying of the stomach, hard to digest components of the diet, usually from vegetables, are retained and accumulate in the stomach. A ball of undigested, plant-derived material can accumulate in the stomach and give rise to symptoms of fullness or can further obstruct the emptying of food from the stomach. Removing the bezoar may improve symptoms and emptying.
A computerized tomographic (CT) scan of the abdomen and upper gastrointestinal x-ray series may also be necessary to exclude cancer of the pancreas or other conditions that can obstruct the emptying of the stomach.
How is gastroparesis treated?
Treatment of gastroparesis includes diet, medication, and devices or procedures that facilitate emptying of the stomach. The goals of treatment include:
To provide a diet containing foods that are more easily emptied from the stomach. Controlling underlying conditions that may be aggravating gastroparesis. Relieve symptoms of nausea, vomiting and abdominal pain. Stimulate muscle activity in the stomach so that food is properly ground and emptied from the stomach Maintaining adequate nutrition. Diet
Emptying from the stomach is faster when there is less food to empty, so smaller, more frequent portions of food are recommended. Soft foods (or preferably liquid) that do not require grinding also are emptied more easily. Moreover, in gastroparesis the emptying of liquids often is less severely affected than the emptying of solids. Fat causes the release of hormones that slow down the emptying of the stomach. Therefore, foods low in fat empty faster from the stomach. In patients with severe gastroparesis, sometimes only liquid meals are tolerated.
Controlling underlying conditions
High levels of glucose (sugar) in blood tends to slow gastric emptying. Therefore it is important to lower blood glucose levels in patients with diabetes to near normal levels with diets and medications. Individuals with a deficiency of thyroid hormone (hypothyroidism) should be treated with thyroid hormone. If bezoars are present, they should be removed (usually endoscopically).
Relieving nausea, vomiting, and abdominal pain
Drugs used to relieve nausea and vomiting in gastroparesis include promotility drugs (see discussion that follows) such as metoclopramide (Reglan) and domperidone, anti-nausea medications such as prochlorperazine (Compazine) and promethazine (Phenergan), serotonin antagonists such as ondansetron (Zofran), anticholinergic drugs such as a scopolamine patch (commonly used for treating motion sickness), drugs used for treating nausea in cancer chemotherapy patients such as aprepitant (Emend), and medical marijuana Marinol.
Drugs used to relieve abdominal pain in gastroparesis include non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Motrin) and naproxen (Aleve), low dose tricyclic antidepressants such as amitriptyline (Elavil), drugs that block nerves that sense pain such as gabapentin (Neurontin), and narcotics such as tramadol (Ultram) and Fentanyl. Narcotic pain relievers as a group tend to cause constipation and slow emptying of the stomach, and, therefore, should be avoided or used with caution among patients with gastroparesis.
Stimulating muscle activity
Oral Drugs. There are four oral drugs that are used to stimulate contractions of the stomach’s muscles, referred to as pro-motility drugs. These drugs are cisapride (Propulsid), domperidone, metoclopramide (Reglan), and erythromycin. Cisapride is an effective drug for treating gastroparesis; however, it was removed from the market because it can cause serious and life-threatening irregular heart rhythms. Despite this fact, it can be obtained for use through the pharmaceutical company that manufactures it (Janssen Pharmaceuticals) under a strictly monitored protocol but only for patients with severe gastroparesis unresponsive to all other measures. Domperidone has not been released for use in the US; however, it can be obtained if approval is obtained for its use from the US Food and Drug Administration. The fourth drug, erythromycin (E-Mycin, Ilosone, etc.), is a commonly-used antibiotic. At doses lower than those used to treat infections, erythromycin stimulates contractions of the muscles of the stomach and small intestine and is useful for treating gastroparesis.
It has been demonstrated that tegaserod (Zelnorm), an oral drug used for treating constipation in irritable bowel syndrome (IBS), increases emptying from the stomach just as it does from the colon. However, in March of 2007, the FDA asked Novartis to suspend sales of tegaserod (Zelnorm) in the United States because a retrospective analysis of data by Novartis from more than 18,000 patients showed a slight difference in the incidence of cardiovascular events (heart attacks, strokes and angina) among patients on Zelnorm compared to placebo. The data showed that cardiovascular events occurred in 13 out of 11,614 patients treated with Zelnorm (.11%), compared to one cardiovascular event in 7,031 (.01%) placebo-treated patients. However, it is unclear whether Zelnorm actually causes heart attacks and strokes. Doctors and scientists will be scrutinizing the data to determine the long term safety of Zelnorm.
Further studies will be necessary to determine just how effective tegaserod is and how it compares to the other medications that are available for treating gastroparesis before its use can be recommended.
There are two important guidelines in prescribing oral drugs for gastroparesis. First, the drugs must be given at the right times, and second, the drugs must reach the small intestine so that it can be absorbed into the body. Since the goal of treatment is to stimulate muscular contractions during and immediately after a meal, drugs that stimulate contractions should be given before meals.
Most drugs must be emptied from the stomach so that they can be absorbed in the small intestine. The majority of patients with gastroparesis have delayed emptying of solid food, and pills and capsules, like solid food, do not empty well from the stomach. As mentioned previously, many patients with gastroparesis have less of a problem emptying liquids as compared with solid food. Therefore, liquid medications usually are more effective than pills or capsules.
Intravenous drugs. Occasionally, patients have such poor emptying of both liquid and solid food from the stomach that only drugs given intravenously are effective. In such patients, intravenous metoclopramide or erythromycin can be used. A third option is octreotide (Sandostatin), a hormone-like drug that can be injected beneath the skin. Like erythromycin, octreotide stimulates short bursts of strong contractions of the muscles in the stomach and small intestine. Due to its greater expense and the need for injection, octreotide is used only when other medications fail.
Electrical pacing. Electrical pacing of the stomach is a new method for treating severe gastroparesis. Electrical pacing of the stomach is analogous to cardiac pacing for the treatment of an abnormally slow heartbeat and involves the placement of a pacemaker. The pacemaker usually is placed laparoscopically and does not require a large abdominal incision for entering the abdomen. During placement, wire electrodes are attached to the muscle of the stomach. The wires are brought out through the abdominal wall just beneath the skin. The wires are attached to a small, battery-operated pacemaker that is buried in a surgically-created pouch just under the skin. The skin is then sutured so that the pacemaker and wires are beneath the skin. The pacemaker generates electrical impulses that are transmitted by the wires to the muscles of the stomach, and the muscles contract in response to the impulses. Electrical pacing is effective in many patients with severe gastroparesis, but the numbers of patients who have been treated is small. Since electrical pacing of the stomach is relatively new, the long-term effectiveness and safety have not been determined clearly.
Surgery. Surgery occasionally is used to treat gastroparesis. The goal of surgery is to create a larger opening between the stomach and the intestine in order to aid the process of emptying the stomach's contents. Alternatively, the entire stomach may be removed. These procedures should be considered only when all other measures have failed because of the potential complications from the surgery. Surgery should be done only by surgeons in consultation with gastroenterologists who are knowledgeable and experienced in caring for patients with gastrointestinal motility disorders (disorders of the nerves or muscles of the gastrointestinal tract that affect digestion and transport of food).
Maintaining nutrition
Patients with mild gastroparesis usually can be successfully managed with pain relievers and pro-motility medications, but patients with severe gastroparesis often require repeated hospitalizations to correct dehydration, malnutrition and to control symptoms.
Treatment options for dehydration and malnutrition include:
Intravenous fluids to correct dehydration and replenish electrolytes if nutrition is adequate but symptoms occasionally interrupt the intake of even liquid food. Enteral nutrition which provides liquid food directly into the small intestine, bypassing the paralyzed stomach. Intravenous total parenteral nutrition (TPN) to provide calories and nutrients (TPN is a fluid containing glucose, amino acids, lipids, minerals, and vitamins—everything that is needed for adequate nutrition—intravenously. The fluid usually is delivered into a large vein via a catheter in the arm or upper chest.) Doctors generally prefer enteral nutrition over TPN because long-term use of TPN is associated with infections of the catheter and liver damage. Infection can spread through the blood to the rest of the body, a serious condition called sepsis. Catheter-related sepsis often requires treatment with intravenous antibiotics and removal of the infected catheter or replacement with a new catheter. TPN also can damage the liver, most commonly causing abnormal liver tests in the blood. TPN-induced liver damage usually is mild and reversible (the liver test abnormalities return to normal after cessation of TPN), but, rarely, irreversible liver failure can occur. Such liver failure may require liver transplantation.
Enteral nutrition is safe and effective. The two common means of delivering enteral nutrition are via naso-jejunal tubes or jejunostomy tubes. The jejunum is the part of the small intestine just past the duodenum, the first part of the small intestine just beyond the stomach. Both naso-jejunal tubes and jejunostomy tubes are designed to bypass the stomach and deliver nutrients into the jejunum where they can be absorbed.
A naso-jejunal tube is a long, thin catheter inserted (usually by a radiologist or a gastroenterologist) via the nostril into the stomach. The tip of the naso-jejunal tube is then advanced past the stomach into the small intestine. Often this must be done during upper GI endoscopy. Liquid nutrients then can be delivered via the naso-jejunal tube into the small intestine. Naso-jejunal tubes generally are safe, but there are cosmetic disadvantages and discomfort of having a tube in the nose. The problems that occur with naso-jejunal tubes are primarily accidental or intentional removal by the patient, blockage of the tube by solidified nutritional solutions, and aspiration (backup of stomach contents into the lungs that can lead to pneumonia).
A jejunostomy is a catheter placed directly into the jejunum. It can be done during standard abdominal surgery, using minimally invasive techniques (laparoscopy), or by a specially-trained radiologist. With a jejunostomy, the catheter passes through the skin on the abdominal wall and directly into the jejunum. Before a jejunostomy is placed, a trial of naso-jejunal nutrition often is given to be certain that the small bowel is not involved with the same motility problem as the stomach and that nutritional liquids infused into the small intestine will be tolerated.
What is the prognosis (long-term outcome) for patients with gastroparesis?
If gastroparesis is caused by a reversible problem, for example pancreatitis, the condition will subside when the underlying problem resolves. In some diabetics, better control of their blood sugar will improve emptying of the stomach. If there is no reversible cause, gastroparesis rarely resolves. In fact, it may become worse with time. Gastroparesis is particularly difficult to treat when there are accompanying motility disorders of the muscles of the small intestine.
What is new in gastroparesis?
The newest experimental treatment for gastroparesis is injection of botulinum toxin into the pylorus. The pylorus is the narrow channel through which food passes from the stomach to the duodenum. The pylorus, like the stomach, is a muscular organ. The pylorus is closed most of the time due to continuous contraction of the pyloric muscle. Intermittently it opens and allows secretions from the stomach to enter the small intestine. After meals, the pylorus is very important for metering the emptying of the stomach. In gastroparesis, although the muscles of the stomach are weak all of the time, the muscle of the pylorus remains strong and contracted and the pylorus relatively closed. It was hypothesized that if the strength of the pyloric muscle was reduced, food might empty from the stomach more readily. Although a surgical procedure, termed pyloroplasty, to enlarge the pylorus has been used in the past to treat problems with emptying of the stomach, it is major surgery and has had mixed results with respect to its efficacy. More recently, relaxation of the pyloric muscles has been produced by injecting botulinum toxin (Botox) into the pylorus. Although results have been good, the procedure has not been studied enough to recommend its use unless it is part of a research protocol.
Gastroparesis At A GlanceGastroparesis is a disease of the muscles of the stomach or the nerves controlling the muscles that causes the muscles to stop working. Gastroparesis results in inadequate grinding of food by the stomach and poor emptying of food from the stomach into the intestine. The primary symptoms of gastroparesis are nausea and vomiting. Gastroparesis is best diagnosed by a test called a gastric emptying study. Gastroparesis usually is treated with nutritional support, drugs for treating nausea and vomiting, drugs that stimulate the muscle to contract, and, less often, electrical pacing and surgery. http://www.medicinenet.com/gastroparesis/page5.htm
Tuesday, August 07, 2007
What is the treatment for dehydration? And what are ways of preventing dehydration?
Just some info I received from one of my gastro docs. I was having a little trouble with the bathroom trotts. Knowing this has led to dehydration and a pancreas flair in the past, I wanted to avoid it if at all possible. I was trying to use OTC Immodium without much luck. So I started with the Poweraid to try and replace the fluid and electrolytes. The doctor explained that sports drinks are not the best way to approach re hydration. Sugar (too much) seems to be the culprit. He referred me to the below article with a home remedy for fluid replacement recommended by the World Health Organization. Please understand that this is not intended to be a cure-all. Dehydration is serious and should be treated by your doctor. The article follows, along with the orig. link: http://www.medicinenet.com/dehydration/page2.htm
What is the treatment for dehydration? And what are ways of preventing dehydration?
The best way to treat dehydration is to prevent it from occurring. If you suspect excessive fluid loss during and illness, your physician should be notified. Intravenous or oral fluid replacement may be needed, depending on severity of fluid loss. In the 1960's the World Health Organization (WHO) developed an oral solution containing sugar, which improved the absorption of salt/water preparations, saving the lives of many dehydrated persons in remote areas. This solution can be prepared at home by mixing the following:
1. Table Salt - 3/4 teaspoon2. Baking Powder - 1 teaspoon3. Sugar -4 tablespoons4. Orange juice - 1 cup5. Water - 1 quart/liter
This beverage can be taken in small, frequent sips, and is often tolerated in the face of nausea and vomiting. Several commercial preparations are available, but since their composition varies, your physician should be contacted to decide which replacement solution (if any) is best. Changes in the type or amount of fluid replacement may be needed as symptoms improve. Care must be taken to avoid using these solutions improperly.
Food intake should be continued if at all possible, except for high fiber fruits and vegetables. There is controversy regarding ingesting milk products since the ability to absorb milk sugar (lactose) may be reduced. The prior policy of "bowel rest" seems to do more harm than good except in certain circumstances.
Saturday, August 04, 2007
Doctors Post By Marmite
REMEMBER 50% of the Doctors graduated in the bottom half of the class.There is ONLY 1 doctor who is BEST in the hospital, State, Country! Then there is always different fields of endeavour.. We go to GI, do you realise that very few specialise in the Pancreas?We go to Surgeons, do you know that very very few specialise in the pancreas.. then there are ones who specialise in roux n y, whipple etc etc. Some are better than others.. Do you know where in the worl dis considered the country of excellence for Pancreas Surgery? India. They have more than 1 billion people, 4 times the pop of the US, so they have more people to operate on.
I have laid in hospital MANY times, A&E way too much and to a lesser extent, wards.I often overhear patients families complaining bitterly that the "doctor SHOULD KNOW .."I have seen people get deathly ill, go to hospital, been admitted, got well, and gone home and NO ONE has any idea what was wrong with them, or how they got better.One lady, on my first trip, couldnt digest food. She could handle "clear soup", cup of black tea or coffee, no problem, but white tea and coffee or cream soup would simply sit there and cause her to bloat. She had a black belt in karate, so she was rather fit and generally healthy. One day they had her scheduled for surgery, she came bac, and the surgeon said "Good news.. it is not cancer!".She was horrified.She asked what it was?? No idea they replied, but it is definitely not cancer!
She got better, and went home, I saw her in hospital a year or two later, same problem and she had lost a lot of weight and condition. I have no idea what has happened since.
You MUST remember that they only perfect diagnostic tool is AUTOPSY, and no one seriously ever wants to go there. Especially not just for a diagnosis.
Celeste and Jerry did 59 dud doctors b4 finding one that worked. You go as far as you have to. You have to put together your MEDICAL TEAM. That includes all of them. Listen to CJ and their experience. Don't stop with anyone who is not the very best, most especially when it comes to surgery.. Panc Surgery is no longer regarded as probably mortal, 30% chance up til the 1990s just from cutting into the pancreas.About that time, I think it was the UK surgeons who decided that only panc accredited surgeons could do scheduled panc surgery. It spread world wide as a std. In emergencies anyone will do what they can to help anyone but if there is panc surgery to do and a panc surgeon is available they lead the team, always!
Again, a great whipple surgeon may be poor on puestow, so check their record. You might wonder how someone gets to be good at something without doing it first, it is the tutor system. If you wanna be a whipple guy, go assist a whipple guy and stand beside him thru all his surgeries, eventually, you will be handed the reigns while he looks over your shoulder.
As the patient or family there of, ASK QUESTIOS. The better the question the greater the respect you develop with your medical practitioner. My GP/PCP at age 60 said he had never seen a case of pancreatitis in General Practice. He vaguely remembered maybe a coupla cases when he was a Reg at the end of his training. he said he had no intimate knowledge, and that he would help but if it were panc related, go to the panc specialist thru the hospital.
When I left my home city to come 200 miles north, for family support, my Panc Surgeon said there was ONLY one guy to talk to here about pancreas here in Welly. Take good advice when it is on offer!
The single most important SECOND thing, after assembling the best medical team you can get no matter what, is to keep the Food & Event diary. This is the greatest diagnostic tool you will ever help with in your particular case. Remember, every panc case is unique and ultimately different to everyone else's! Write down everything you did and ate in the 6-12-24 hours prior to you attack or episode.This is CRITICAL to determining if you contributed to your upset condition. AND you probably did. Many foods do contribute or are even the prime cause of attack. Alcohol is probably the #1, Stress is probably the #1, physical movements are probably the #1, Hot Spice is probably the #1, find out what your #1s are, and avoid them at all costs. Antibiotics were a surprise to me, but they can hurt hurt you. Cold is another one that upsets me, food acid, [apples/tomatoes], all sorts of thiungs will contribute to setting you off. One hospital admission was due to 3 tomatoe sandwiches, I never found this out til 18 months later when a support group meeting tossed this up as a trigger for another person.
I can't speak highly enuff of support groups for pancreatitis. Simply sitting down with other people and telling them how bad that pain was, the horror of the way I live, and they were able to nod sagely and say " I know how that feels"! THAT was special. That is after a long time having A&E doctors and nurses abusing me, frequently, nurses in wards doing the same thru basic ignorance, and lo9tsa people not understanding the condition, me or my particular levels of discomfort with this horrible affliction.
I have never said or posted the word disease. I use affliction, it seems a lot more powerful and nasty. Disease seems to me as a rash, or creeping minor nastiness even if it is severe like leprosy. I don't think it is a BAD enuff word to describe what my pancreas does to me! AFFLICTION, I am afflicted by this damnable medical condition!
Take this seriously, it can kill you. Chronic Pancreatitis will not kill you, but it will destroy your additional organs, liver, kidneys, lungs, heart and lots more. The F&E diary is vital in helping you work out things to do to lower the misery you go thru. It is not a complete solution but it can stop a lot of things starting. As described elsewhere, things like stress can hardly be avoided sometimes. I remember watching the World Trade Centre atrocity unfold live on TV and the stress levels rose, instantly. Simply seeing something as bad as that was translated into pain readily. Stress in everyday life thru family and friends can't be avoided, and that can put you in hospital. Identify every thing in your life which is aggravating your panc condition and then avoid them like the plague.
Talk to family, friends and workmates about your condition and how it effects your everyday life. Tell them things they can do to help or not hurt you, and encourage them to understand you and what exactly you are going thru.
I know my own family never really believed me when I told them what was happening to me and how bad it was. Even when I moved closer to them, they still never really understood, but with time and them doing my total shopping etc, they have come to be my best defenders and they isolate me as much as possible from any and all situations that can hurt me. Namely they deal with all govt departments and hospital administration. They drive me to all doctors visits and come in with me. They help me write out all the questions and points I want to raise and make sure those points are covered as well as writing down answers so I can discuss these with them later if I have missed things.
I no longer function at a high level. I have short term memory problems. I can remember things from school in full detail but can't tell you what happened last week, or even things I agreed to do. I figure this is cos my life is so bland, with no changes, that I don't have points that stand out as different or unique. I only know it is weekend cos the TV programs are different. I don't watch much TV but it is on all the time I am awake, it provides me with human type company while I am alone, which is the way of things except for twice a week. I have a cleaning lady that comes in once a week and my brother and sister come over once to just talk about whatever happens to come up. Life has changed a lot since I was a cab driver dealing with a hundred different people every day!
Stay in control of your life. Do what it takes to monitor you version of this affliction. Inform others about your plight, and ask good questions of your medical team, it will improve your relationship with them.
KEEP your attitude as best you can, positive and be open to suggestions, no matter where they come from. Don't let anyone tell you how to feel or behave, only you can KNOW this. Speak up for yourself, or do what I do, have your family speak for you to insulate yourself from idiots and arseholes, they are everywhere, including hospitals and especially in govt departments.
Have a pain managed day!
This is posted as written by the Author
Tuesday, June 26, 2007
Liverpool Hospital Link
The link posted above should be bookmarked by all of us. Never mind where you are treated, and as I did with Dr Sutherland, you simply email the head sharang and you will get answers and assistance.
You owe it to yourself to have access to the latest in the world of Panc Research and this is one place you can get it..
BOOKMARK IT NOW!!!
Liverpool Uni - Pancreas
Wednesday, April 11, 2007
Links from Alma
Lorie,I should have just posted the link below for those needing info on chronic pain. This link will take you to the forms you may want to print out and take to your dr. I keep the one where there is just a drawing of the human body in my wallet along with my medical history. This way all I have to do is hand it to the dr or nurse. It sure helps to have it filled out before seeing a dr or being admitted to the clink because usually when you are in bad pain you have a hard time trying to describe the pain. This scale will provide it for you.http://www2.rpa.net/~lrandall/index.html
Follow Ups:
Posted by Alma on August 05, 2006
Celeste,Do you think we could add this to the link at the bottom of this page and/or to the blog Brett is working with? I think it pertains to some of the issues many of us have and I am also thinking of how it would help this particular organization to be read by other viewers.
http://www.myida.org/index.html
http://www.myida.org/index.html
Posted by Alma on August 11, 2006
I know some of you are trying to get your social security disability. I found these links on the IDA web site and thought you might could use them.
Social Security Disability Advocate - USAdvocates.org - nationwide legal representation for SSA disability issues.http://www.usadvocates.org/
Free 1-on-1 Disability Case Evaluation - Free Attorney Disability Eval. Law Office of Stephanie Joy, Esq. No Fee until you get your benefits. Quicker Results, Higher Success Rate. 1-on-1 with Attorney. All 50 states. Ssdi, SSI.http://www.sojlaw.com/
Free Social Security Disability Help - How to win your social security disability case - The Social Security Disability Resource Site. Have an experienced attorney contact you for a free consultation about your case.http://www.4socialsecuritydisability.com/
Lorie Bledsoe web site
I wanted to let everyone know that my new website is up and running. My Sister KXXXX has built a beautiful site for me to share my Story, journaling, Pictures and Testimonials that my family and friends have written to me. I have been through a lot of kleenex!There are links to my Doctor's and just ton's of information that we keep adding to daily. I want to shout it from the roof tops. If I can get it out there in front of hundreds of people then maybe just maybe I can help someone. I would love to keep anyone from having to endure the pain I have went through. I know you all know and I am sure many of you have the same feelings. My family will journal daily when I have my TP/ICT so each and everyone of you that are interested can follow my journey to hopefully a new life of pain free years. If any of you want to pass it on please do! I have been struggling lately with anxiety and a lot of pain and nausea. The thing that keeps me going right now is the hope of a new life and sharing my journey so I can be a voice for the people that are unable to. The support of friends and family means the world to me right now! Thank You for that! Lorie http://www.supportloriebledsoe.com/
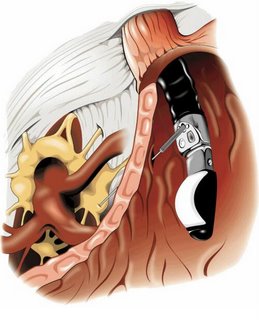
New System more precise than ERCP?
Researchers reported at the DDW (Digestive Disease Week) meeting in Los Angeles, that direct visualization with a device called SpyGlass™ altered their diagnosis or treatment strategy with most patients who had been previously examined with ERCP.Data shows that up to 30% of diagnostic ERCP are inconclusive, potentially creating the need for further testing. ‘Direct visualization significantly improves the chances of accurately diagnosing and treating a patient in one procedure, thus achieving the full potential of ERCP’, stated lead investigator Yang K. Chen, MD, from the University at Colorado at Denver and Health Sciences Center. Both bench simulation and animal testing showed that the SpyGlass system to be effective for access, direct visualization and biopsy in all bile duct quadrants. Furthermore, this procedure can be performed by a single operator, as compared to conventional systems where two operators are required. In this investigator initiated first human use experience and bench simulation study, the researchers used the SpyGlass system to examine and treat 22 patients with various disorders. According to DDW co-presenter Douglas Pleskow, MD, Colon Cancer Center, Beth Israel Deaconess Medical Center, Boston, Mass., ‘the use of SpyGlass altered the initial ERCP impression and ultimately changed patient treatment strategy in 19 patients.’ To overcome the limitations of conventional ERCP, this new system uses a miniature 6,000-pixel fiber optic SpyGlass probe that attaches to the camera head. The probe is inserted through a single-use access and delivery catheter that can be steered in four directions to access and inspect all four quadrants of the treatment area. The system attaches directly to a standard duodenal scope. The SpyGlass system is manufactured by Boston Scientific Corporation. The company’s Senior Vice President, Steve Moreci, summed up the results by saying that ‘These studies indicate that the SpyGlass Direct Visualization System has the potential to redefine how ERCP is performed and to potentially help physicians obtain a more accurate diagnosis quickly.’
Dr's Oath..First Do No Harm
Friday, April 06, 2007
Port-A-Cath
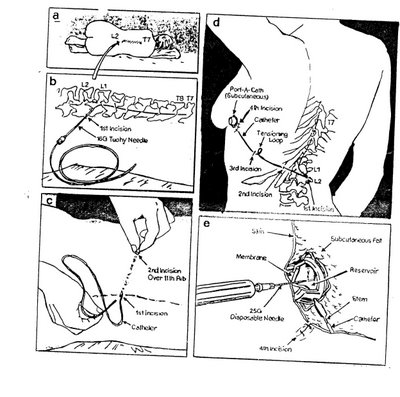

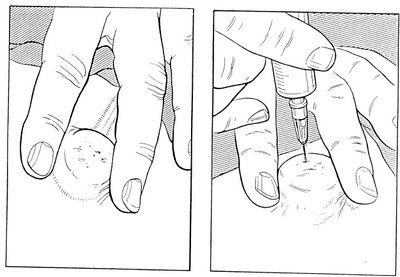
On the 25th of June I am going to have a Port-A-Cath inserted in my spine. Below is the information and Diagrams that I have received in preparation for this. What this will enable me to do is deliver very small doses of lignocaine or narcotic medication directly to my spine therefore eliminating my pain. I will have to inject every 4 or so hours . This will then let me wean myself off my narcotic medication and control my pain during this process. The Dr’s believe if I then stay off the narcotic medication for a little while I will be able to restart the same medication and get a much better result or a significantly lower dose. It will be as if I had never taken the drug before. They may leave the port in place for as long as it is working and causing no problems. Up to 5 years.
Tuesday, August 22, 2006
My Pain is my prisoner
It makes me to lie down between hospital sheets
It destroyeth my soul:
It loses me in the paths of sickness, I’m sick of its name Even tho I walk down the hospital corridors is till fear evil,
Tho my drip is with me its pole and its bad don’t comfort me
They prepare others tables in the presence of my nausea
They assault my body with drugs, my patience runs out.
Surely illness and despair will leave me and I will dwell in this house of sickness no MORE!!
This was posted on the PMB with a request to find out who the orginal Author was. So if you can help then please feel free to post a comment. Thanks for your help.
Wednesday, August 02, 2006
What does S.O.D. Stand for?
In Reply to: ps. what does sod stand for? posted by jeff on July 24, 2006 at
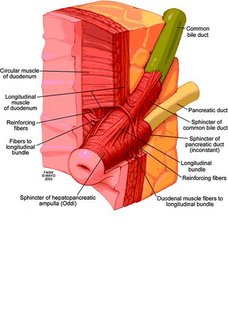
Sphincter of oddi disfunction.. its also on jerrys blog.. I'll put the pic here and then paste the info in this post**************************************************
This is a picture that shows the sphincter of oddi. the main pancreatic duct and bile duct from the liver both converge and their liquids are released via the sphincter. The main pancreatic duct will back up with activated enzymes and they will eat and destroy all along the length of the pancreas. In the torso diagram, where the head of the pancreas is (torsos right side) Jerry has a knot that protrudes out of his abdomen. We were todl that the pancreas is swelling so large that it pushes out from under the stomach and that is what is causing the bulge.*******************************************
ps the bulge is gone and has not returned! so it was the pancreas and NOT a food bolus!
Insurance Help Sites
Patient assistance programs-helpingpatients.org/
--------------------------------------------------------------------------------
www.togetherrxaccess.com/
www.medicare.gov
www.disabilityresources.org To find disability organizations or agenices in your area, click on your home state:
http://www.ncpad.org/organizations/alpha
http://www.focusas.com/HealthInfoNumbers.htm Toll-Free Numbers for Health Information
http://www.3m.com/us/healthcare/pha...ssistance.jhtml
http://sis.nlm.nih.gov/hotlines/
http://coveringkidsandfamilies.org/communications/bts/
http://www.freemedicineprogram.com/drug/ELDER+TONIC/
http://www.mycancernews.com/viatical.html
http://www.cancercare.org/HelpingHa...deList.cfm?c=49
http://www.helpingpatients.org/
http://www.rxassist.org/default.cfm
http://www.doctorhealthynet.com/fre...dicine_home.htm
http://www.needymeds.com/
http://www.mhsanctuary.com/add/rx.htm
http://www.astrazeneca-us.com/content/drugAssistance/
https://www.merck.com/pap/pap/consu...application.jsp
http://www.pfizer.com/subsites/phil...ents.index.html
http://www.sch-plough.com/schering_...nt_programs.jsp
http://www.phrma.org/
http://www.hrsa.gov/osp/dfcr/obtain/obtain.htm
http://www.lillyanswers.com/
http://www.benefitscheckup.com/
http://www.pharma.us.novartis.com/i...?TNav&checked=y
Bristol Stool Scale

Bristol Stool ScaleFrom Wikipedia, the free encyclopediaYou have new messages (last change).Jump to: navigation, search
The Bristol Stool Scale or Bristol Stool Chart is a medical aid designed to classify the faeces form into seven groups. It was developed by Heaton and Lewis at the University of Bristol and was first published in the journal Scand J Gastroenterol in 1997. Because the form of the stool depends on the time it spends in the colon, there is a correlation between the colonic transit time and the stool type.
The seven types of stool are:
Type 1: Separate hard lumps, like nuts (hard to pass)
Type 2: Sausage-shaped, but lumpy
Type 3: Like a sausage but with cracks on its surface
Type 4: Like a sausage or snake, smooth and soft
Type 5: Soft blobs with clear cut edges (passed easily)
Type 6: Fluffy pieces with ragged edges, a mushy stool
Type 7: Watery, no solid pieces (entirely liquid)
Types 1 and 2 indicate constipation, with 3 and 4 being the "ideal stools" especially the latter, as they are the easiest to pass. 5-7 being further tending towards diarrhoea.
[edit]ReferencesConstipation Management and Nurse Prescribing: The importance of developing a concordant approach PDF Faecal incontinence and constipation PDF [edit]External linksThe Bristol Stool Scale from Medscape.com Information from Solvay Pharmaceuticals Childhood Constipation Retrieved from "http://en.wikipedia.org/wiki/Bristol_Stool_Scale"Categories: General practice | Gastroenterology
Ambry Test
http://www.ambrygen.com/reports/Pancreatitis%20Sales%20Aid%205-06.pdf
The Ambry Test : PancreatitisPancreatitis is a serious problem with asignificant genetic component.Pancreatitis accounts for 87,000 hospitalizationsper year in the US.1 Chronic pancreatitis patientsface a 26-fold increased risk of pancreatic cancer,and for those with hereditary pancreatitis, the riskis 50-fold with approximately 40% developingpancreatic cancer by age 70.2Normal exocrine pancreatic function depends on adelicate balance of enzyme activation andinhibition which can be affected by multipleenvironmental and genetic factors. Hereditarypancreatitis has been linked to mutations in thePRSS1 gene. Study of idiopathic chronic andrecurrent acute pancreatitis demonstrates thatmutations in three genes – PRSS1, SPINK1, andCFTR – predispose to pancreatitis.3Due to the cumulative contribution of three genesin both dominant and recessive patterns, a patientmay have genetically-determined pancreatitis evenif family history is negative.Ambry Genetics offers the world’s onlycomprehensive genetic test for pancreatitis.To help determine etiology and suggestappropriate treatments, Ambry Genetics offersanalysis of all coding regions of the CFTR, PRSS1,and SPINK1 genes in The Ambry Test: PancreatitisAMPLIFIED™. This test also analyzes the CFTRgene for gross deletions and duplications, whenindicated, providing a detection rate ofapproximately 99% for each gene. The panel isalso available without CFTR deletion/duplicationanalysis (The Ambry Test: Pancreatitis, CFdetection rate 97-98%), and each test is availableseparately.100 Columbia #200 | Aliso Viejo, CA 92656 | 949 900 5500fax 949 900 5501 | toll free 866 262 7943 |
www.ambrygen.com|
Pancreatitis1 in 4 patients tests positive for at least onesignificant genetic mutation.Mutations in three genes predispose to chronicand recurrent acute pancreatitis:• CFTR – cystic fibrosis transmembraneconductance regulator• PRSS1 – cationic trypsinogen• SPINK1 – serine protease inbitor, Kazal type 1Genetic testing for pancreatitis can help you:• Avoid repeated diagnostic testing• Provide targeted therapy• Address increased cancer risk in geneticallydeterminedpancreatitis• Help your patient understand his condition andincrease compliance• Communicate inheritance risks tofamily membersNo other test can identifymore mutations thanThe Ambry Test:Pancreatitis AMPLIFIEDGet started with Ambry Genetics today.Sample submission kits are available atno charge. Please call 866-262-7943 or visitour website to obtain more information andall necessary forms.™100 Columbia #200 | Aliso Viejo, CA 92656 | 949 900 5500fax 949 900 5501 | toll free 866 262 7943 | www.ambrygen.com|
Pancreatitis• In the entire patient set, 49.1% (116/236) carriedat least one mutation.• 11.0% (26/236) had a form of CF confirmed by2 CF mutations. An additional 22.0% (52/236)had one CF mutation.• 8.9% (21/236) had mutations in more than one gene.• Only 4.2% (10/236) patients had PRSS1mutations only.• Approximately 1/4 patients (23.7%, 56/256) havemutations with a clear causative component(defined as presence of 2 CF mutations and/orknown deleterious PRSS1 or SPINK1 mutations).83891, 83894, 83898,83903, 83904, 83909,839123-5 WeeksFull gene mutation scanning is performed by modified TemporalTemperature Gradient Electrophoresis (mTTGE). All sequencevariations detected by mTTGE are identified by double-strandedautomated sequencing. If indicated, CFTR gross deletion /duplication testing is performed by MLPA (MRC Holland).Blood: 5cc peripheral blood in purple-top EDTA (preferred) oryellow top ACD. Store at 2-8° C up to 96 hours prior toshipping. Do not freeze. Ship at room temperature.CPT CodesTurn-Around-TimeMethodSpecimenRequirements1 Yakshe P. Pancreatitis, chronic. emedicine [online resource]. Available at: http://www.emedicine.com/MED/topic1721.htm. Last update July 2005.2 Erickson RA. Pancreatic cancer. emedicine [online resource]. Available at: http://www.emedicine.com/MED/topic1712.htm. Last update Dec 2005.3 Etemad B, Whitcomb DC. Gastroenterology. 2001;120:682-707.4 Whitcomb DC.US Gastro Review. 2006;56-58, and personal communication.© 2006 Ambry Genetics. All rights reserved. P0506-09-003-MKG-00.PANCREATITIS PANEL PANCREATITIS PANEL AMPLIFIED83891, 83894, 83898, 83900,83901, 83903, 83904, 83909,839124-6 Weeks1 in 4 patients has at least onesignificant mutation.In a series of patients with chronic or recurrentacute pancreatitis, The Ambry Test: Pancreatitisdetected at least one mutation in 49.1% (116/236).Though patients known to have cystic fibrosis (CF)were excluded from this series, 11.0% (26/236) werefound to have a form of CF confirmed with at leasttwo CFTR mutations. Nearly as many patients(8.9%, 21/236) had mutations in more thanone gene.Using a stricter definition of clinical significance aspresence of known deleterious mutations in PRSS1or SPINK1, and/or two CF mutations, approximatelyone in four patients (23.7%, 56/236) has a causativegenetic component to their pancreatitis.Genetic testing results can help youmanage your patient.As mutations in different genes affect differentsteps of trypsin activation and inhibition, genetictesting can suggest treatments targeted to apatient’s particular defect. For example, PRSS1mutations may lead to premature trypsinogenactivation through altered sensitivity to calcium.Preventive measures could include various steps tominimize stimulation of the acinar cells and assistcalcium regulation.4 CFTR mutations impairpancreatic duct flushing, so treatments could focuson stimulating the pancreas and maximizing flowthrough the duct.4Identifying patients with mutations allowsappropriately increased cancer surveillance.Knowledge of contributory mutations explains thedisease to the patient, reinforces understanding ofits chronic nature, and affirms the importance ofcompliance with dietary and lifestyle modifications.Further, family members may be tested andcounseled to minimize their risk of developingchronic pancreatitis.Mutation distribution in 236 patients testedwith The Ambry Test: Pancreatitits
The Ambry Test : PancreatitisPancreatitis is a serious problem with asignificant genetic component.Pancreatitis accounts for 87,000 hospitalizationsper year in the US.1 Chronic pancreatitis patientsface a 26-fold increased risk of pancreatic cancer,and for those with hereditary pancreatitis, the riskis 50-fold with approximately 40% developingpancreatic cancer by age 70.2Normal exocrine pancreatic function depends on adelicate balance of enzyme activation andinhibition which can be affected by multipleenvironmental and genetic factors. Hereditarypancreatitis has been linked to mutations in thePRSS1 gene. Study of idiopathic chronic andrecurrent acute pancreatitis demonstrates thatmutations in three genes – PRSS1, SPINK1, andCFTR – predispose to pancreatitis.3Due to the cumulative contribution of three genesin both dominant and recessive patterns, a patientmay have genetically-determined pancreatitis evenif family history is negative.Ambry Genetics offers the world’s onlycomprehensive genetic test for pancreatitis.To help determine etiology and suggestappropriate treatments, Ambry Genetics offersanalysis of all coding regions of the CFTR, PRSS1,and SPINK1 genes in The Ambry Test: PancreatitisAMPLIFIED™. This test also analyzes the CFTRgene for gross deletions and duplications, whenindicated, providing a detection rate ofapproximately 99% for each gene. The panel isalso available without CFTR deletion/duplicationanalysis (The Ambry Test: Pancreatitis, CFdetection rate 97-98%), and each test is availableseparately.100 Columbia #200 | Aliso Viejo, CA 92656 | 949 900 5500fax 949 900 5501 | toll free 866 262 7943 | www.ambrygen.com| Pancreatitis
1 in 4 patients tests positive for at least onesignificant genetic mutation.Mutations in three genes predispose to chronicand recurrent acute pancreatitis:• CFTR – cystic fibrosis transmembraneconductance regulator• PRSS1 – cationic trypsinogen• SPINK1 – serine protease inbitor, Kazal type 1Genetic testing for pancreatitis can help you:• Avoid repeated diagnostic testing• Provide targeted therapy• Address increased cancer risk in geneticallydeterminedpancreatitis• Help your patient understand his condition andincrease compliance• Communicate inheritance risks tofamily membersNo other test can identifymore mutations thanThe Ambry Test:Pancreatitis AMPLIFIEDGet started with Ambry Genetics today.Sample submission kits are available atno charge. Please call 866-262-7943 or visitour website to obtain more information andall necessary forms.™100 Columbia #200 | Aliso Viejo, CA 92656 | 949 900 5500fax 949 900 5501 | toll free 866 262 7943 | www.ambrygen.com| Pancreatitis•
In the entire patient set, 49.1% (116/236) carriedat least one mutation.• 11.0% (26/236) had a form of CF confirmed by2 CF mutations. An additional 22.0% (52/236)had one CF mutation.• 8.9% (21/236) had mutations in more than one gene.• Only 4.2% (10/236) patients had PRSS1mutations only.• Approximately 1/4 patients (23.7%, 56/256) havemutations with a clear causative component(defined as presence of 2 CF mutations and/orknown deleterious PRSS1 or SPINK1 mutations).83891, 83894, 83898,83903, 83904, 83909,839123-5 WeeksFull gene mutation scanning is performed by modified TemporalTemperature Gradient Electrophoresis (mTTGE). All sequencevariations detected by mTTGE are identified by double-strandedautomated sequencing. If indicated, CFTR gross deletion /duplication testing is performed by MLPA (MRC Holland).Blood: 5cc peripheral blood in purple-top EDTA (preferred) oryellow top ACD. Store at 2-8° C up to 96 hours prior toshipping. Do not freeze. Ship at room temperature.CPT CodesTurn-Around-TimeMethodSpecimenRequirements1 Yakshe P. Pancreatitis, chronic. emedicine [online resource]. Available at: http://www.emedicine.com/MED/topic1721.htm. Last update July 2005.2 Erickson RA. Pancreatic cancer. emedicine [online resource]. Available at: http://www.emedicine.com/MED/topic1712.htm. Last update Dec 2005.3 Etemad B, Whitcomb DC. Gastroenterology. 2001;120:682-707.4 Whitcomb DC.US Gastro Review. 2006;56-58, and personal communication.© 2006 Ambry Genetics. All rights reserved. P0506-09-003-MKG-00.PANCREATITIS PANEL PANCREATITIS PANEL AMPLIFIED83891, 83894, 83898, 83900,83901, 83903, 83904, 83909,839124-6 Weeks
1 in 4 patients has at least onesignificant mutation.In a series of patients with chronic or recurrentacute pancreatitis, The Ambry Test: Pancreatitisdetected at least one mutation in 49.1% (116/236).Though patients known to have cystic fibrosis (CF)were excluded from this series, 11.0% (26/236) werefound to have a form of CF confirmed with at leasttwo CFTR mutations. Nearly as many patients(8.9%, 21/236) had mutations in more thanone gene.Using a stricter definition of clinical significance aspresence of known deleterious mutations in PRSS1or SPINK1, and/or two CF mutations, approximatelyone in four patients (23.7%, 56/236) has a causativegenetic component to their pancreatitis.Genetic testing results can help youmanage your patient.As mutations in different genes affect differentsteps of trypsin activation and inhibition, genetictesting can suggest treatments targeted to apatient’s particular defect. For example, PRSS1mutations may lead to premature trypsinogenactivation through altered sensitivity to calcium.Preventive measures could include various steps tominimize stimulation of the acinar cells and assistcalcium regulation.4 CFTR mutations impairpancreatic duct flushing, so treatments could focuson stimulating the pancreas and maximizing flowthrough the duct.4Identifying patients with mutations allowsappropriately increased cancer surveillance.Knowledge of contributory mutations explains thedisease to the patient, reinforces understanding ofits chronic nature, and affirms the importance ofcompliance with dietary and lifestyle modifications.Further, family members may be tested andcounseled to minimize their risk of developingchronic pancreatitis.Mutation distribution in 236 patients testedwith The Ambry Test: Pancreatitits
Celiac Plexus Block
In Reply to: Celiac Plexus Nerve Blocks posted by Robin H. on August 01, 2006 at 10:42:48:
(image placeholder)
I knew someone on here had had something diff done. Thats why i told jeff, someone else will pipe up with info. also i found this neat page!!
*****************************************************ROUND TABLE
Article in PDF format - JOP Home page
JOP. J Pancreas (Online) 2004; 5(4):315-321.
Celiac Plexus Neurolysis
Paolo Giorgio Arcidiacono, Marzia Rossi
Diagnostic and Therapeutic Endosonography Unit, Division of Gastroenterology and Gastrointestinal Endoscopy, Vita-Salute San Raffaele University - San Raffaele Hospital. Milan, Italy
Introduction
Pancreatic cancer is the tenth most common malignancy and the fourth cause of cancer-related death in Western countries. Because 5-year survival in referral centers is less than 30%, clinical management of most patients involves palliation of the symptoms of which 90% are weight loss, jaundice, and pain.
While jaundice related to biliary obstruction can be palliated by means of endoscopic therapy or surgery, pancreatic pain is often difficult to control.
Initial therapy with non-steroid anti-inflammatory agents (NSAIDs) is often rapidly overwhelmed by pain and necessitates being associated with opioid administration.
Although opioids effectively relieve pain, they are associated with many different collateral effects, such as dry mouth, constipation, nausea, vomiting, drowsiness and delirium, which can determine a great decrease in quality of life and may also impair the immune function. Pancreatic pain is also quite common in patients with chronic pancreatitis and, in this case, pain has a multi-factorial etiology; for this reason, prolonged drug therapy is related to an increased risk of narcotic-dependence [1].
Celiac plexus neurolysis (CPN) is a chemical splanchnicectomy of the celiac plexus; its goal is to ablate the efferent nerve fibres which transmit pain from the intra-abdominal viscera.
Although the terms "celiac plexus" and "splanchnic nerves" are often used interchangeably, these are anatomically distinct structures.
The splanchnic nerves are located above the diaphragm (retro-crural) and are typically anterior to the 12th thoracic vertebra; on the other hand, the celiac plexus is situated below the diaphragm (ante-crural), surrounding the basis of the celiac trunk. This plexus is composed of a dense network of ganglia and interconnecting fibres (Figure 1).
Figure 1. The celiac plexus.
The ganglia vary in number (1-5), size (diameter 0.5-4.5 cm), and location (T12-L2), but, independently on their size, the ganglia cannot be visualized as distinct structures by any kind of imaging modality.
The celiac plexus transmits pain sensation originating from the pancreas and most of the abdominal viscera except for the left colon, rectum and pelvic organs.
Stimuli reach the thalamus and the cortex of the brain, leading to pain sensation. On the contrary, some descending inhibitory mechanisms may also modulate the ascending pain information.
The CPN technique was first described by Kappis et al. in 1919 [2]; since then, a number of modifications have been proposed and introduced in a clinical setting in an attempt to improve the accuracy of needle placement and pain relief while reducing procedure-related complications.
Nowadays, CPN is most commonly used to palliate patients suffering from pain due to pancreatic cancer and chronic pancreatitis; it can be performed using different approaches either percutaneously, surgically or under EUS guidance. Until the 1990s, the most common of the above was surely the percutaneous route, injecting absolute alcohol into the celiac plexus under fluoroscopy or CT guidance.
Different studies have reported data on safety, accuracy in reaching the right site of injection and efficacy in decreasing pain due to different diseases by means of CT-guided CPN.
Some authors described 28 cases of CPN performed under CT guidance in patients having neoplasms originating in the pancreas (n=10), stomach (n=8), bile ducts (n=5), liver (n=3), right colon (n=1) and kidney (n=1) [3]. The study showed that this procedure is safe and efficient in controlling pain [3].
Unfortunately, the CT CPN approach is usually posterior and, for this reason, cases of paraplegia have been reported caused by the puncture of the nervous radix at the time of the introduction of the needle during the procedure [4].
Endoscopic ultrasonography (EUS) is a relatively new imaging technique which couples a high frequency ultrasound probe with an oblique viewing endoscopic instrument. This combination allows the endoscopist to obtain a perfect evaluation of the pancreatic parenchyma and surrounding structures, not least, the aorta and celiac trunk. This imaging modality has achieved wide acceptance as the technique of choice for the evaluation of pancreatic disease, diagnosis and staging of pancreatic cancer, diagnosis of idiopathic pancreatitis and the evidencing of neuro-endocrine neoplasms.
At the beginning of EUS, instruments were provided by radial scanning probes; this means that the scanning plane of these probes was transversal, that is, perpendicular to the longitudinal axis of the endoscopic instrument.
This probe orientation absolutely limited the possibility of these instruments performing EUS guided diagnostic or therapeutic procedures, due to the inability of the probe to follow, under real time guidance, the route of a needle device from the orifice of the working channel of the EUS instrument to a target lesion located either inside the gut wall or, as for CPN, outside the gut wall. In early 1990s, there was a technical revolution in EUS instrumentation; in fact, a longitudinal echoendoscope was presented.
This instrument was made with an electronic convex high frequency probe having a longitudinal scanning plane; this means that the scanning plane was on the same longitudinal axis as the endoscope and, more importantly, on the same axis of the working channel.
This innovation has opened the field of operative EUS, allowing the possibility of following, under real time guidance, any kind of device passed throughout the working channel to reach a target lesion.
Since that time, EUS has been tested in this new operative setting for many reasons, mainly the cytological analysis of tumors and, more recently, it has been applied in the treatment of pain in patients with chronic pancreatitis or pancreatic cancer by injecting neurolytic agents in the area of the celiac plexus.
Although many studies demonstrate that celiac plexus neurolysis effectively controls pancreatic cancer pain, up to 1% of patients undergoing percutaneous CPN may develop serious complications, including lower extremity weakness, paresthesias, including epidural anesthesia, lumbar puncture and pneumothorax.
In theory, EUS CPN is safer than posterior percutaneous techniques because EUS allows direct access to the celiac plexus without risk to the vital spinal nerves, the diaphragm or the spinal arteries.
Procedure
EUS-guided celiac plexus neurolysis (EUS CPN) is usually combined with the biopsy of a pancreatic primary lesion for diagnostic and staging purposes. It is performed with a linear array echoendoscope (Figure 2).
Figure 2. Linear array echoendoscope.
With these instruments, it is possible to follow, under EUS real time guidance, the route of the needle through the pancreatic lesion.
Informed consent is obtained with specific attention to complications associated with CPN and EUS guided fine needle aspiration (FNA) of pancreatic lesions. The procedure is performed under deep sedation under the supervision of an anesthesiologist. The patient lays on left lateral decubitus and his/her vital parameters are monitored.
Under direct endoscopic view, the linear EUS instrument is introduced into the stomach to reach the lesser curve in the sub-cardiac area. In this position, the probe is lightly pressed against the gastric wall to obtain a good coupling and a good view of surrounding structures. At this site, it is easy to identify the aorta under the diaphragm which appears as an anechoic tube structure in a longitudinal plane and the origin of the celiac axis is seen beside this. Color Doppler can confirm the vascular landmarks (Figures 3 and 4).
Figure 3. Monochrome visualization of the celiac trunk.
Figure 4. Color Doppler visualization of the celiac trunk.
As previously emphasized, the celiac plexus is not identified as a discrete structure but is located based on its position relative to the celiac trunk.
Two different treatment procedures have been described to perform EUS CPN depending on the device used to perform alcohol injection.
The first technique described uses a standard 22 gauge needle used for all the biopsy procedures under EUS guidance (Figure 5); this is a cutting needle with a removable inner sheet occluding a single hole at the needle tip. For this reason, it is necessary to perform two injections of alcohol at both sides of the trunk in order to obtain an adequate injection of alcohol at both sides of the celiac trunk.
Figure 5. Standard 22 gauge needles.
The second procedure, which is actually more diffused due to its rapidity, uses a new needle (Figure 6) properly designed for this procedure (EUS 20 CPN, Wilson Cook, Winston-Salem, NC, USA); it is a 20 gauge needle with a penetrating tip closed and with some lateral holes which allow a radial diffusion of alcohol to both sides of the origin of the celiac axis with a single injection.
Figure 6. EUS 20 CPN (Wilson Cook, Winston-Salem, NC, USA) needle.
Once the origin of the celiac trunk is located from the sub-cardiac position, the needle (whichever used) is passed through and fixed to the celiac trunk by a luer-lock. Then, under real time control, the needle is released and pushed out from the working channel to trans-pass the gastric posterior wall and is immediately inserted adjacent to the celiac trunk.
At this phase, the two procedures differ slightly, considering the needle position with respect to the celiac trunk; in the first procedure, due to the fact that the needle has only one hole and cannot spray alcohol, the needle tip is positioned by one side of the trunk originating from the aorta and, after having completed the injection, it must be pulled back slightly and again inserted on the other side of the trunk to carry out another injection.
In the second technique, the spraying possibility given by the EUS 20 CPN needle allows the endosonographer to put the needle tip anterior to the basis of the origin of the celiac axis and to carry out only one injection (Figure 7).
Figure 7. EUS image of the needle at base of the celiac trunk.
The injection time is identical for both devices used. When the needle tip is in place, the inner sheet is removed and an aspiration test is performed to rule out vessel penetration before injection.
Then, 3-6 mL of a local analgesic, usually bupivacaine 0.25-0.75%, is injected first followed by 15-20 mL of a neurolytic agent (98%) dehydrate alcohol (Figure 8).
Figure 8. EUS image of lidocaine injection.
The alcohol injection produces an echogenic cloud obscuring the aorta and celiac axis (Figure 9).
Figure 9. EUS image of alcohol injection showing an echogenic cloud obscuring aorta and celiac axis.
In chronic pancreatitis patients, some Authors prefer to use steroids (10 mL or 80 mg (6 mL) triamcinolone) instead of alcohol.
However, in chronic pancreatitis, most results are obtained with alcohol and when traditional techniques were used.
The EUS CPN procedure usually lasts approximately 15 minutes and, during the procedure, arterial pressure has to be monitored because the alcohol injection may produce hypotension and it is necessary to infuse saline solution.
Results
Currently, there are few data about CPN under EUS guidance. However, the results are comparable to other conventional methods used to relieve pancreatic pain with neurolytic agent injections.
The safety and efficacy of EUS CPN has previously been demonstrated as relieving pancreatic pain in a cohort of 25 patients with pancreatic cancer followed for 12 weeks and 5 patients with other intra-abdominal malignant neoplasms [5]. These studies showed a significant decrease of pain at 2, 4, 8 and 12 weeks after EUS CPN.
About 80% of the patients also benefited in a long-term observation (a mean follow up-of 10 weeks) [5]. Other Authors described 58 patients treated in order to palliate pain due to non-operable pancreatic cancer. A short-term decrease of pain was seen in 78% of the patients but the control of pain decreased in 30% at 12 weeks.
Of particular interest is the evidence, reported by Gunaratnam et al. in the widest population reported to have been treated using this modality, that, if the treatment is associated with chemoradiation or chemotherapy, the decrease in the pain score was significantly higher as compared to patients who did not undergo any additional therapy [6] (Figure 10).
Figure 10. Decrease of the pain score according to different treatments. (N Gunaratnam et al. [6], modified).
Up to now, the real role of EUS CPN in the treatment of pain related to chronic pancreatitis is not so clear, lacking enough comparative data comparing EUS CPN and other modalities of treating such multifactorial pain.
Only two studies [7, 8] have tested EUS CPN in this setting; in 90 patients steroids were injected during EUS CPN and a beneficial effect was observed after 7 days in only 55% [7]. Furthermore, in the follow-up of these patients, only 25% still showed a significant decrease in the pain score after 12 weeks [7].
Many authors believe that the difference in results between patients with pancreatic cancer or chronic pancreatitis probably depends on the origin of the pain which can be considered only due to the nervous growing of the tumor in pancreatic cancer and which is multifactorial, with a great psychological impact, in chronic pancreatitis.
Another study described 22 cases of CPN (10 EUS CPN and 12 CT CPN) which showed the benefit in 40% at 8 weeks under EUS guidance (30% at 24 weeks) and in 25% under CT guidance. But the Authors concluded that the number of patients was too limited [8].
There are only a few complications related to the procedure and they are described as only transitory [3]. Orthostatic hypotension or a transient diarrhea may frequently be described.
The infusion of liquid can contrast the hypotension, while the diarrhea is generally auto-limiting and does not exceed 24 hours. Only a few cases of chronic diarrhea have been described; other complications are: peri-pancreatic abscess, reversible paraparesis and a pseudo alcohol-induced aneurysm [9, 10, 11]. To prevent the abscess, it is important to carry out antibiotic prophylaxis.
Conclusions
Celiac plexus neurolysis during EUS appears to be a safe technique, without complications. It seems to control neoplastic pancreatic pain in a short time in about 90% of cases and in a long time in about 30%.
In the management of chronic pancreatitis pain, the role of EUS CPN is not so clear and only 50% of patients have a good reduction of pain within a short period of time. However, only 10% seem to show a benefit at 24 weeks. EUS CPN results seem to be comparable to the results obtained with the other procedures, although the numbers are still too low. An important advantage is that EUS CPN may be performed during bioptic staging of pancreatic cancer [12].
It is also not very clear if there is the possibility of performing more than one procedure of neurolysis.
In summary, EUS CPN is safe and effective for the palliation of patients with pain caused by unresectable pancreatic cancer. Chemotherapy with and without radiotherapy also significantly decreased pain scores.
In addition, the proximity of the posterior lesser curve of the stomach to the celiac plexus, the use of continuous real time visualization of the target area and the availability of the Doppler to assess the vasculature all facilitate accurate needle placement.
CPN under EUS guidance requires further investigation in order to identify the advantages of this approach over conventional percutaneous techniques. The ability to perform the procedure in conjunction with tumor staging and FNA may streamline the care of these patients. The use of EUS CPN earlier in the course of pancreatic cancer to alleviate pain should be encouraged.
References
Levy MJ, Wiersema MJ. EUS-guided celiac plexus neurolysis and celiac plexus block. Gastrointest Endosc 2003; 57:923-9. [More details]
Kappis M. Sensibilitat und lokale Anasthesie im chirurgischen Gebiet der Bauchhohle mit besonderer Berucksichtigung der splanchnicus-Aasthesie. Beitrage zur klinischen Chirurgie 1919; 115:161-75. [More details]
Lee JM. CT-guided celiac plexus block for intractable abdominal pain. J Korean Med Sci 2000; 15:173-8. [More details]
Eisenberg E, Carr DB, Chalmers CT. Neurolytic celiac plexus block for treatment of cancer pain: a meta-analysis. Anesth Analg 1995; 80:290-5. [More details]
Wiersema MJ, Wiersema LM. Endosonography-guided celiac plexus neurolysis. Gastrointest Endosc1996; 44:656-62. [More details]
Gunaratnam NT, Sarma AV, Norton ID, Wiersema MJ. A prospective study of EUS-guided celiac plexus neurolysis for pancreatic cancer pain. Gastrointest Endosc 2001; 54:316-24. [More details]
Gress F, Schmitt C, Sherman S, Ciaccia D, Ikenberry S, Lehman G. Endoscopic ultrasound-guided celiac plexus block for managing abdominal pain associated with chronic pancreatitis: a prospective single center experience. Am J Gastroenterol 2001; 96:409-16. [More details]
Gress F, Schmitt C, Sherman S, Ikenberry S, Lehman G. A prospective randomized comparison of endoscopic ultrasound- and computed tomography-guided celiac plexus block for managing chronic pancreatitis pain. Am J Gastroentero. 1999; 94:900-5. [More details]
Chan VW. Chronic diarrhea: an uncommon side effect of celiac plexus block. Anesth Analg 1996; 82:205-7. [More details]
Navarro-Martinez J, Montes A, Comps O, Sitges-Serra A. Retroperitoneal abscess after neurolytic celiac plexus block from the anterior approach. Reg Anesth Pain Med 2003; 28:528-30. [More details]
Kumar A, Tripathi SS, Dhar D, Bhattacharya A. A case of reversible paraparesis following celiac plexus block. Reg Anesth Pain Med 2001; 26:75-8. [More details]
Varadarajulu S, Wallace MB. Applications of endoscopic ultrasonography in pancreatic cancer. Cancer Control 2004; 11:15-22. [More details]
Article in PDF format
--------------------------------------------------------------------------------
Keywords Celiac Plexus /innervation; Endosonography; Pain; Pancreatic Neoplasms
Abbreviations CPN: celiac plexus neurolysis
CorrespondencePaolo Giorgio ArcidiaconoDivision of Gastroenterology and Gastrointestinal EndoscopyUniversity Vita-Salute San RaffaeleIRCCS San Raffaele HospitalVia Olgettina, 6020132 MilanoItalyPhone: +39-02.2643.2145Fax: +39-02.215.2559E-mail address: arcidiacono.paologiorgio@hsr.it
JOP Home page
- http://www.joplink.net/prev/200407/26.html
Blood Work Questions
Posted by cj on
In Reply to: blood work question?? posted by jeff
Lab Studies:
Blood tests
**Elevations of serum amylase and lipase are found only during acute attacks of pancreatitis, usually early in the course of the disease**In the later stages of chronic pancreatitis, atrophy of the pancreatic parenchyma can result in serum
enzyme levels within the reference range, even during acute attacks of pain.
While low concentrations of serum trypsin are relatively specific for advanced chronic pancreatitis, they are not sensitive enough to be helpful in most patients with mild-to-moderate disease.
Laboratory studies to identify causative factors include serum calcium and triglyceride levels.
When common etiologies are not found, research protocols are available to test for genetic mutations in cationic trypsinogen and CFTR.
Fecal tests
Because maldigestion and malabsorption do not occur until more than 90% of the pancreas has been destroyed, steatorrhea is a manifestation of advanced chronic pancreatitis, and neither qualitative nor quantitative fecal fat analysis can detect early disease.
Assays of fecal chymotrypsin and human pancreatic elastase 1 have the same limitations but are useful in confirming advanced chronic pancreatitis with exocrine insufficiency.
Pancreatic function tests
Direct tests: These tests are the most sensitive and can be used to detect chronic pancreatitis at its earliest stage; however, they are somewhat invasive, labor intensive, and expensive.
Determination in duodenal aspirates: Intubation of the duodenum usually is performed with a Dreiling tube, which allows for separate aspiration of gastric and duodenal contents. The methodology varies depending on the specific laboratory; however, the authors generally use exogenous secretin with cerulein or cholecystokinin to achieve maximal stimulation of the pancreas. The output of pancreatic bicarbonate, protease, amylase, and lipase then is measured in the duodenal aspirates. This test currently only is available in specialized centers. While the greatest sensitivity can be obtained in prolonged infusions of secretagogue to uncover a decreased pancreatic secretory reserve, it is impractical for general clinical use.
Determination in pancreatic juice: This test generally is performed in conjunction with an endoscopic retrograde cholangiopancreatography (ERCP). The pancreatic duct is freely cannulated, an exogenous secretagogue is administered as above, and the pancreatic juice then is aspirated out of the duct as it is produced. The output of pancreatic bicarbonate, protease, amylase, and lipase are measured. This test is gaining popularity because most patients undergo ERCP at some point in their evaluation.
Indirect tests: Noninvasive tests of pancreatic function have been developed for detecting chronic pancreatitis. In principle, these tests work via oral administration of a complex substance that is hydrolyzed by a specific pancreatic enzyme to release a marker substance. The intestine absorbs the marker, which then is measured in the serum or urine. These tests are capable of detecting moderate-to-severe chronic pancreatitis. The presence of renal, intestinal, and liver disease may interfere with the accuracy of these tests. Neither currently is freely available in the
http://www.emedicine.com/med/topic1721.htm
Monday, June 12, 2006
Gary Fry


On April 30th 2006 Gary Fry passed away leaving behind his much loved wife Rhonda who’s battles with Chronic Pancreatitis was the inspiration for the creation of the Pancreatitis Message Board(PMB). Gary didn’t just create a great place where you posted a message, he created a family atmosphere and welcomed unreservedly anyone who wanted to post and make themselves known. The sense of family and community has always been a special feature of this board and through this Gary helped so many people who suffer pancreas related problems many of whom may never have actually made a post on the board but read often. He also kept it going through some very hard times but he had enough compassion/kindness in him to realize how much the many members of the community he had created depended on his board and he chose never to give up on it. Gary you are much loved and will be sorely missed,
I struggled to write about what Gary meant to the many people who frequent the PMB. So the best way I could think of was to take a selection of the many posts and e-mails that accompanied the sad news of Gary’s death.
From Alma
I first met Gary in the mid to late 90’s. I had been diagnosed with chronic pancreatitis in 1995 and was playing around on the computer learning how to navigate the internet. I found a site made by a person by the name of Bruce. His site was nothing but pancreas information and stories. I cried like a baby when I read the stories of others who had chronic pancreatitis. It was like finally someone could to relate and understand what I was going through. There was a link to other sites on Bruce’s site and I went through all of them. On one of the links I clicked on I immediately knew I had found a safe haven. I emailed Gary and we emailed each other back and forth and he had a message board he had started so his wife Rhonda could have someone to talk with that knew what she was going through. It was like we clicked immediately as friends. On the first message board there was not a lot of us and what there was instantly felt like family members that had known each other all their lives.
Gary showed me how to make a web site using a site on the internet that helps you do it. I still had questions and he would help me with them. I learned a lot from Gary not only about message boards and web pages but about life in general. His wife was very ill quite often but he never once complained to me about it. He always wanted to be there for her and was always there for her.
Another thing that brought Gary and myself together is a common love for Bluegrass Music. We both loved the bluegrass sound so we not only had pancreatitis in common but we were both country hicks and we loved this style of music. I even sent him a tape one time of a song I sang to get him to let me know how I was doing. He was honest and helpful. I never will be a true singer but he saw and understood that singing Southern Gospel which includes some bluegrass music, was for me a way to worship my God. Not many people understand that but Gary did from the beginning.
We contacted each other every day for some reason or another, be it me learning how to make web pages or dealing with the pain of cp or just a friendly chat to pass the time. We quickly became like brother and sister. We had our ups and downs like siblings also but we never ever gave up on each other. I will miss him terribly as I know his family will too. Family came first with him and he loved Rhonda with all his heart and more if it was possible. He was ever mindful that Mike could be sent to Iraq and worried about that a lot in the past couple of yrs.
Gary was always supportive of those that posted on the message boards he made. He did not put up with arguing and many times I myself would get in trouble for posting in an argumentative way. Being a very close friend did not stop him from scolding me either. Most times he scolded me in a private email and I really appreciated him for that. He was our rock of Gibraltar when we needed him to be and I don’t see how the board will function without him. I know it will never be the same with him gone. I never dreamed in a million years he would pass on before I did because I was the one with pancreas problems not him. It was a huge shock to find out he had died. Although I had not heard much from him lately I will miss him terribly. Just knowing he was there should I want to email him gave me a sense of security. That security is gone now and there will never be another Gary Fry for me nor will any of the message boards I see on the internet compare in any way to Gary’s board. In honor of him we are keeping the board he made up and running. It is different from other message boards on the internet in the fact that it is not censored. You can say what you want within reason and we all feel like one big family. The board has gotten larger each year and that is because Gary allowed it to be a family oriented board without having to have passwords and approval of a post, etc. I will always hold near to my heart the memories of Gary and his love for Rhonda and Bluegrass Music.
"THANK YOU GARY FOR YOUR CREATION OF THIS BOARD AND LOVE AND SUPPORT YOU HAVE GIVEN ALL OF US."
“It hasn't been easy I know, but you kept right on doing what you could to inform anyone who needed information about chronic pancreatitis. You will never be forgotten.”
Alma
aka: firstwin
Posted by Cindy on May 08, 2006
Taken from an e-mail from Gary to Cindy this was sent to me as is shown here:
“This group is the first to have a Pancreatitis specific message board on the internet. It is the longest running Pancreatitis specific message board as well. I started it in June of 1997 on a different server than it is now. We have moved several times due to different circumstances., usually the server shutting down.”
From Gary’s Sister DiAnn
“I have something that you may like to read about him. It will definitely give you and idea what kind of person he was . He worked in the coal mines and when there was an explosion he was there more than once to help and at times it got pretty gruesome.”
“In 1997 while he was going to college he was one of two people to receive a scholarship called the Felton Patton Memorial Scholarship”
The people on the Pancreatitis were an extended family to him and when we talked he often talked about the people on the board as if I should know them. I did get to the point that I felt like I knew some of them….”.

The excerpt on the right is from the paper clipping below
Subject: Re:Official Resignation as Administrtaor - CJ (c.j.) is new Administrater.
From: Gary
To: All
Date Posted: 21:12:15 12/14/05
Message:
“Wow ALma; I don't know where to start! It has been a two way street, we have been there for each other I think. We probably have been more like family, because we, as many do not know, have had our own ups and downs, (very few and nothing really serious), behind the scene and off the board. But like family, we have always healed our wounds and been able to forgive each other and go forward and leave the past behind. But most of all we were there for each other through the very tough times and we laughed a lot at the good times. I think we have even laughed at our self sometimes :)……”
Posted by Larry on May 02, 2006
I just received an email from Mike Fry who stated his father, Gary Fry, passed away this passed Sunday. If this is true, it is truly a very sad moment for all of us.
Can someone else verify this for us? There was an email address in the email that I received that I may respond back to.
I apologize if this seems so blunt, but I really did not know Gary was doing so bad.
Posted by Chuck on May 02, 2006
I just called the information line at Hampton Funeral Home in Barbourville. Gary Lee Fry did indeed die on Sunday. His funeral will be held Thursday at 1 PM.
I am so sorry to confirm the notice from his son. Gary was a very special person. He put his heart and soul into starting and running this board when Rhonda first was diagnosed. He has been a good friend and will be sorely missed.
Rest in Peace, Buddy.
Chuck
Posted by Brett on May 03, 2006
“Rhonda if you are reading this then please accept my condolences. Gary was a special person who has had a huge impact in my life by providing this special place. For that I am eternally grateful and forever in his debt. I can only imagine the pain you are in and hope that you will find peace for yourself.”
Rest in peace Gary, you will be missed
Posted by Pete on May 03, 2006
“I am truly saddened by Gary's untimely passing. He corresponded with me quite often when I joined this board in July'04.I will be forever grateful for him starting this board.Rhonda...if you read this, please accept my heartfelt sympathies for your loss. You will be in my prayers. I know Gary will be watching over us now from above. God has a special plan for him. I am truly going to miss him...a fine measure of a man!”
Pete(Fla.)
Posted by Christine on May 03, 2006
“i just want to offer my deepest condolences to Gary’s wife and family. i am so grateful to him for all his hard work with this board. it has been a life saver and he has made a difference in so many peoples lives that are suffering with this. i am so, so sorry. thank you Gary, rest in peace.“
Posted by Trisha on May 03, 2006
“What can i say that's not already been said. My thoughts and prayers go out to all his family and friends.I don't honestly know were i would be today if i never found this message board. Gary has helped everyone of us and that say's something about a person.
Rest in peace Gary......Thanks.”
Posted by Pam on May 03, 2006
“My sympathies as well. I saw that Gary last posted on 4/18...he seemed uplifted that this board was active. I hope that gave him joy and peace.”
Pam
Posted by Diane on May 03, 2006:
"REST IN PEACE... a special thank you for this board Gary... from those that post and those that come here as I do to, just read and learn. You and this board have given so much to those who suffer from this horrid disease. Deepest regrets to Rhonda and all that love you."
Diane
Posted by Christine Stanborough on May 03, 2006:
“RhondaTo say Gary was special is such an understatement. God bless you Rhonda your loss is immense and I just hope that our words give you some comfort. You and your family are in our thoughts and prayers.”
Kind regardsChristine
Posted by laurie on May 03, 2006:
“I just want to add my condolences to his family and friends. I am also shocked and profoundly saddened. I missed his posts but took it for granted that he was always going to be here to keep in touch with his legacy.
As far as the board goes with Carol....I think because it was his decision to dedicate this board to her memory that it should be respected. I think that it is a tribute to the person he was that he did this and to change it now would somehow not honour his wishes. Unless of course, there are other issues that his family wish to address. Just my thoughts, such as they are....”
laurie
Posted by Vickie on May 03, 2006:
.”Gary, we've had many conversations down the years and you've been a wonderful friend”
Vickie
Posted by judylu on May 03, 2006:
“I only hope he is at peace now. My heart goes out to Rhonda and the rest of his family and friends. He is surely missed and will be remembered well.”
Posted by Tami on May 04, 2006:
“I found this board in September of last year, and it has been my salvation with this disease. To find so many other people that can truly relate and sympathize as to what you are going through is not only priceless, but very much needed. Gary is and always will be a true hero to me, to stand so vigilantly by his wife’s side during her illness, to offer so much support and knowledge to others going through CP, what a true saint. Rhonda, I don't know you personally, but I am very sorry for what you are going through, your husband loved you so very much and you could just hear it in every word he had to say about you. You and your family are in my prayers, and I will pray for strength during this very difficult time.”
Tami McClurg
Posted by Lorie on May 03, 2006:
“I did not want to come on the board this morning, I waited 2 hours for fear of knowing that Gary has passed away. My heart hurts and goes out to Rhonda and all of Gary's family. Rhonda if you are reading the board please know that my heart goes out to you. I would like for you to know how much Gary has meant to me. Gary was my salvation in 1997 when I found the Pancreatitis message board. I felt alone and confused over my disease. I had so many questions, fears and needed desperately to know what all of this meant and if anyone else was feeling what I was feeling. My husband is supportive, but I don't know that anyone can imagine how we all feel unless you actually walk in our shoes.Gary brought all of us together as a family, none of us would even know each other if Gary had not brought us together with this board. For this we will always remember Gary and for me he will always hold a very special place in my heart. I can't even begin to say everything I am thinking right now. I am still so very shocked. Rhonda you more then anyone knows how much Gary loves you, he is one the most supportive husbands I know he always talked about you with so much love in his heart.Gary, and his passion for music brought joy to many lives. Gary, will be missed greatly. He had a way of sharing his passion's in life through the web. I know God has a plan for him and he is looking over all of us
Rest in peace Gary, Rest in peace.
My condolences to all of Gary's Family.”
Lorie Bledsoe
From CJ
I came across "
From Cindy
“Cant even express to Gary/Rhonda how much the creation of the board has meant to me. Like the rest of you know having this condition that those that don’t have it just can’t understand you 100% and what going thru. This place to come-the board has become over the years with some like extended family to me and to my son Brandon even if we live states/country away like we are so close. I have gained some good friends thru this board including Gary and if it wasn’t for him that would never be-we would have never been brought together for a life of friendship. And one day when Brandon is older and knows/understands my condition and friends over the years he will know about 'Uncle Gary' as well.
Gary you will be missed”
Cindy M
Posted by Cindy on May 08, 2006:
“I came on the board/around since 99. As a lot of you know being the first later on to get pregnant with CP and a lot of you went thru each step with me especially the ups and downs and when I was in the hospital 1 1/2 months while pregnant. For me I would like something said for Gary having to do with that and what he wrote to me when he resigned from board to only be a user of it because some of you called yourselves/I called you 'aunt/nana' and him Uncle Gary he said to Brandon which shows the closeness, caring etc. He called me in the hospital too and helped me with some ?s and worries I had, always included him on emails w/pictures of brandon growing up now 2 1/2 + and he always wrote back such nice things but this one I found hits home and even the part for us to be there/help CJ he knew and went thru some rough times with the board and stuck it out/did what he had to do and best for the board up till when he felt he had to resign. Gary/Uncle Gary -you will be missed tremendously”
Cindy and Brandon
Posted by Gary on December 17, 2005 at 13:02:49:
Cindy;“You, I will never forget. You will always be our first member to deliver a baby, little Brandon, in our group of Pancreatitis sufferer's here. You have always and will always be a friend. Say hello to Brian and little Brandon. Keep in touch. And most of all, lets all help C.J., it is a pretty rough job at times”.
Gary
Finally this was posted by Joan and I thought it was a great way to finish
Posted by Joan on May 12, 2006
I ran across this poem today and when I read it made me think of Gary so I thought I would share it with you guys....
THE BROKEN CHAIN
We little knew that morning that God was going to call your name.
In life we loved you dearly; in death we do the same.
It broke our hearts to lose you, you did not go alone;
for part of us went with you, the day God called you home.
You left us peaceful memories, your love is still our guide;
and though we cannot see you, you are always at our side.
Our family chain is broken, and nothing seems the same;
but as God calls us one by one, the chain will link again.
Author Unknown
Sunday, June 11, 2006
Medical Malpractice
The legislation would create a "one size fits all" system for people injured in a medical setting or nursing home. The limits would apply no matter how severe the harm - even if the wrong limb was amputated, an unnecessary mastectomy was performed, or even in cases involving the death of a child. Congress has their priorities mixed up. Shouldn't we be talking about protecting the health and safety of patients, rather than protecting Congress' corporate friends in the health care, insurance and HMO industries.Urge Congress to oppose any legislation seeking to restrict the rights of people through so-called medical malpractice "reform."
http://www.thepetitionsite.com/takeaction
/991264371?z00m=88688&z00m=88688<l=1149961706